More Anti-VEGF Injections Might Increase Visual Acuity
STOCKHOLM: Retrospective data analysis conducted in the real world revealed that higher improvements in visual acuity were linked to the administration of more anti-VEGF injections over a 5-year period for the treatment of macular edema caused by retinal vein occlusion (RVO). The study team came to the conclusion that this showed the need for longer-lasting therapies and ongoing observation in order to preserve vision.
At the American Society of Retina Specialists (ASRS) 2024 Annual Meeting, the results were presented.
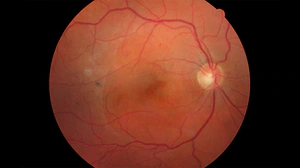
RVO is the second most frequent retinal vascular condition, according to Christiana Dinah, MBBS, MRes, London North West University Healthcare NHS Trust, London, United Kingdom. RVO is a substantial cause of visual impairment. Future projections indicate that its prevalence will rise as a result of aging populations and an increase in cardiovascular disease.
“We know that there is very limited data in terms of the long-term outcomes with treatment of retinal vein occlusion,” she stated. “Our study analyzed the anti-VEGF treatment patterns for macular edema secondary to retinal vein occlusion in the UK and visual outcomes in this population over 5 years.”
The Study
Researchers analyzed Medisoft electronic health record data from 2013 to 2023, gathered by 16 UK National Health Service trusts, for this retrospective, observational analysis.
Patients with macular edema due to hemi-RVO (HRVO), central RVO (CRVO), or branch RVO (BRVO) were included in the study. Inclusion criteria: patients had to have had visual acuity assessed at index injection, at least one intravitreal anti-VEGF injection given on or after diagnosis, and follow-up for three to sixty months following index injection.
The analysis comprised 3511 eyes from 3465 patients with BRVO and 3568 eyes from 3514 patients with CRVO or HRVO. After the index injection, more than half (57.4%) of the eyes were observed for at least 24 months, and 19.1% were observed for up to 60 months.
In the initial half-year, BRVO eyes were administered an average of 4.3 anti-VEGF injections, while CRVO and HRVO eyes were administered an average of 4.1 injections. This suggests a high treatment frequency during this early stage.
In contrast, BRVO eyes had an average of 2.1 injections, while CRVO and HRVO eyes received an average of 2.0 injections throughout the next six months. The average number of injections has been falling over time. BRVO and C/HRVO eyes received 3.4 and 3.2 injections in the second year of follow-up, respectively, and 2.5 and 2.4 injections in the fifth year.
More Is Better
The changes in visual acuity were also monitored; at three months after injection, there was a mean improvement of 11.1 Early Treatment Diabetic Retinopathy Study letters for BRVO and 13.8 letters for CRVO and HRVO. By month sixty, the mean improvement had dropped to 8.3 and 7.0 letters, respectively.
“We saw rapid and substantial visual gain within 3 months,” she stated. “Until around 18 months ago, when it began to decrease, this remained stable. By year five, the visual gain in the CRVO group is at least half of what it was at the beginning.”
The researchers saw less increases in visual acuity in those who had fewer injections. The low (< 4), medium (4–8), and high (> 8) injection groups’ mean changes at month 12 revealed the following trend: According to Dinah, there is a correlation between higher injection numbers and better visual outcomes. This highlights the significance of persistent treatment in maximizing vision recovery.
Elucidating Results With a Caveat
One of the study’s main limitations, according to Yasha S. Modi, MD, a vitreoretinal surgeon at New York University in New York City who moderated the Retinal Vascular Disease Symposium 2 panel discussion at ASRS24, is the loss of follow-up data.
He questioned how selection bias affected the interpretation of the results, saying, “When you have the data looking at 3500 patients to start and then by 60 months you are down to 500 patients, you only have about 15% of your original data set.”
“We have to take these results with that caveat,” Dinah stated. The results of the study, she continued, should be interpreted in light of the fact that randomized control trials have demonstrated that patients who receive injections every 4–8 weeks, as opposed to every 3 months, experience greater visual gains. “That suggests that the number of injections does matter, and we need more durable treatments to maintain the initial vision gain.”



